Conversations on Compassion Fatigue is a new series where we interview professionals from high-stress and trauma-exposed environments and discuss issues around compassion fatigue, organizational health, vicarious trauma, moral distress and self-care.
In this first installment, we sit down with a Mental Health Advocate to discuss her real world experience of compassion fatigue on the job.
Can you describe to us what you do as a Mental Health Advocate?
“My day-to-day has a lot of variety but most of my time is spent talking on the phone and meeting with patients, their families and/or their substitute decision maker. I speak with them to ensure that they know their rights, their liberties and to help them to understand what is happening in terms of their treatment plan. My job is to support the patient and advocate for their wishes concerning what medications they take, what procedures they under-go, etc.
I work separately from the staff at the various hospitals that I visit throughout the region. This is a deliberate model so that I can take my patients’ issues forward to the hospitals without the fear of repercussions that, say a nurse or doctor, may face in a similar situation.
Many of my clients I work with have experienced many obstacles throughout their life; childhood trauma, poverty, unsafe housing,etc.
People who struggle with mental health issues can be very vulnerable – and the medical staff have huge power over their patients (and often rightly so). However, by the time my patients and their families end up with me, they have had years of bad things happening to them and are very angry at the system. I often hear things like – “Why is this happening to me?”
I also do quite a bit of public speaking in my job – ensuring that new and in-coming staff have education around patients’ rights.”
Have you heard about compassion fatigue before?
“Learning about compassion fatigue was, for me, a real light bulb moment. I first encountered the term during a workshop at an annual staff training. I was new on the job – just a few years in – when I first learned about it.
A big take away for me was the idea that “if you have compassion, you will have compassion fatigue.” It was also really helpful to learn that compassion fatigue was a normal experience.
I used to think to myself “How do people get so mean?”,“You didn’t start off by being awful to your patients – so what happened?” Now I see compassion fatigue all over the place.
I think the problem is that, if there isn’t a culture of supporting or recognizing that compassion fatigue happens, it can fester. I’ve seen this manifest in the form of disrespect and staff being dismissive of the people that they are here to care for. If this culture is left unchecked, it can start to taint even the “good” staff.
Learning about compassion fatigue has also been really helpful for me in situations when I’m dealing with staff. It helps keep me from “getting on my high horse” about things. I have more empathy towards the staff. It helps me to re-frame the situation and keeps me from dehumanizing them (which is interesting since that “dehumanizing” is what caused the situation in the first place).”
Have you personally experienced compassion fatigue in your work?
“Absolutely. There was a time in my life when a bunch of things had happened – not just work-related. But I was so tearful and I remember always making the excuse of going to the bathroom just to get a break. Anything would set me off.
I did go for counselling but found the experience to be unsatisfactory. Overtime things got better as I paid more attention to my self-care. However, the experience bothered me because of how it manifested. I felt so weak. It was frustrating.”
What does your self-care practice look like? Has your work encouraged you to do self-care?
For self-care, I take it solely upon myself. My work pays lip service to it, but it really is up to me. I am, however, lucky that my manager is incredibly accommodating. If I needed to take time off, I could.
In my down time I love to run and I play piano too.
Another thing that helps me is to find the humour in things – even though the work that I do is serious, there are moments that can be quite funny. I look for those.
I also collect quotes – those really help me.
I do think that work-life balance is a bit of myth – it always seems to be skewed one way or the other.
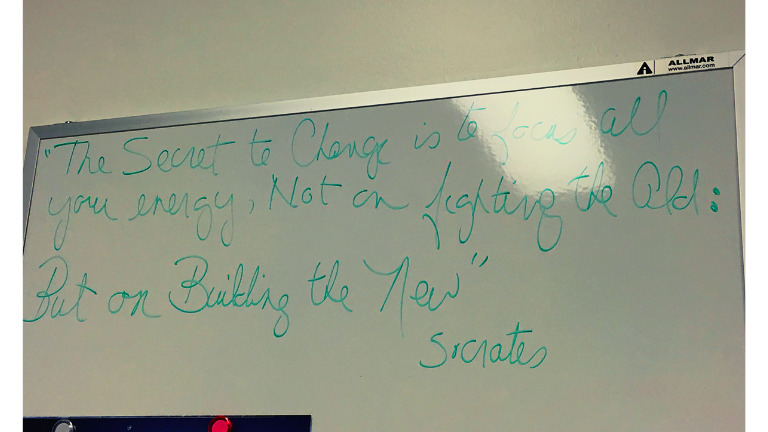
Photo of a quote in her office. It reads: “The Secret to Change is to focus all your energy – Not on fighting the Old: But on Buildling the New – Socrates”
In your field, what do you think could be done to help mitigate the effects of compassion fatigue?
“Oh I have lots of ideas for this! *laughs*
One thing that I think would be really effective is to have a rotation system for front-line staff. This way, staff wouldn’t be seeing the same people over and over again, year after year. Everyone needs a change of pace.
The idea that you’re stuck in one place for the rest of your career is really hard. Perhaps we could move people to research projects, professional development, etc. This would give everyone a break – including the patients.”
What do you find challenging about your work?
“My job is to advocate and act on what the patient wants – not what I think is the best decision for the patient. This can be really hard when I know that a certain medication or treatment would really benefit them – however, as much as I wish I could help them, that’s not my job.
Another thing that can be hard with this job is navigating the barriers in the system. So, here’s a small example and one that happens a lot – I wish that I could give my clients a drive. Sometimes it will be miserable outside and we’re going to the same place, however, due to liability issues, I can’t offer them a ride. I feel so bad about that.”
What do you find rewarding about your work?
When you do work that you feel is meaningful, you don’t realize how much you grow along with it. After doing this work, I’m so different from who I used to be.
Even though it can be challenging, my job is a blessing. I consider myself to be very lucky. Speaking with my patients and being even a small part of their life is such a privilege.”
Are there any resources you would recommend?
“I highly recommend the work of Dr. Patricia Deegan.”
You can find a list of Dr. Deegan’s work here.
Selected articles:
Deegan, P.E. (1996). Recovery as a Journey of the Heart. Psychiatric Rehabilitation Journal 19, 3, p. 91–97. [PDF available here, provided by the Toronto CMHA]
Deegan, P.E. (1988). Recovery: The lived experience of rehabilitation. Psychosocial Rehabilitation Journal, 9, 4, 11-19. [PDF available here, provided by the Toronto CMHA]
1 Comment
Comments are closed.
High Quality content